Betalin Therapeutics, an Israeli biotechnology company specializing in diabetes treatments, recently announced the development of a new technology called Engineered Micro Pancreas (EMP) that enables the secretion of significant levels of glucose-regulated insulin over long periods of time.
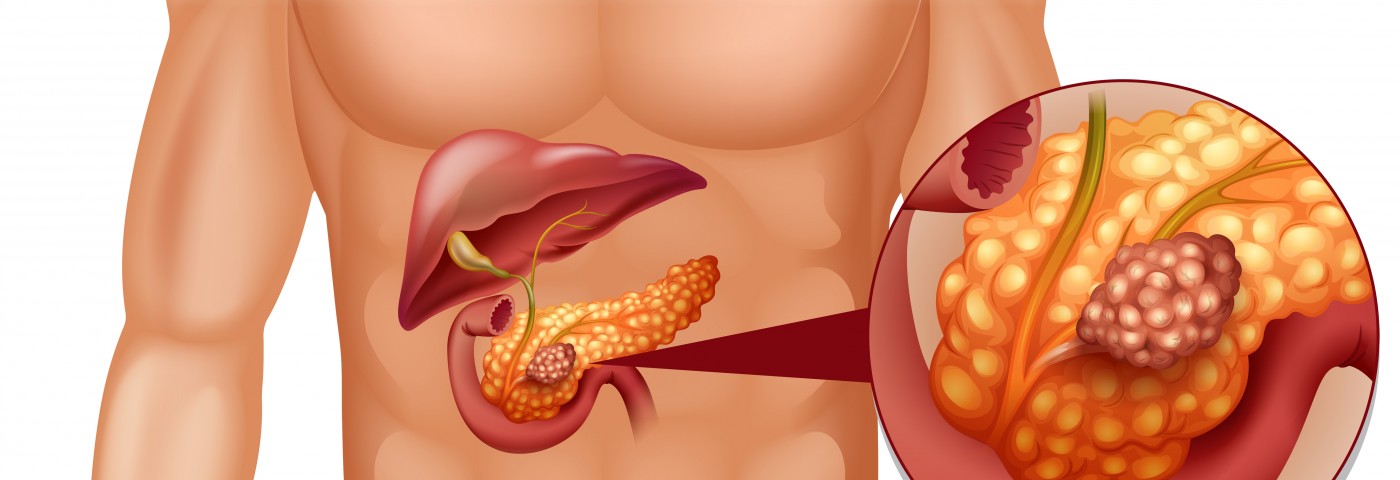
Type 1 diabetes is an autoimmune disease where the beta cells (cells that produce, store and release insulin) of the pancreas are attacked by the body’s own immune system. A transplant of pancreatic islets containing beta cells is a therapeutic approach taken for some patients with type 1 diabetes whose blood-sugar levels are difficult to control. The transplant is made from a deceased organ donor, and the islets are collected, purified and processed in the laboratory, and then transferred to the recipient.
Usually, the recipient receives two infusions with about 400,000 to 500,000 islets per infusion. Once the islets are implanted in the patient, the beta cells begin the production and release of insulin. However, pancreatic islet transplantations are a limited treatment for reasons that include the two separate infusions, the considerable number of cells required, and that fact that the majority of the transplanted cells die within a short timeframe (usually two days). Furthermore, 50% of the patients who undergo such transplantation are still insulin-dependent one year after the procedure, and only around 10% of the patients remain insulin-independent five years after transplantation.
The Betalin Therapeutics’ EMP strategy was designed with the idea that beta cells will only function properly if they have an appropriate connective tissue scaffold to ensure their long-term survival. The technology allows the development of organ-derived micro-scaffolds with a natural architecture and the same basic connective tissue composition, and guarantees that every cell is close to a source of essential gases and nutrients.
A study based on the EMP technology was recently published in the journal Tissue Engineering Part A, showing that beta cells derived from human islets in EMPs function in a similar way to freshly dissected pancreatic islets in vitro. The study is entitled “Beta Cells Secrete Significant and Regulated Levels of Insulin for Long Periods when Seeded onto Acellular Micro-Scaffolds.” Furthermore, researchers also show that beta cells in EMPs secrete insulin in a regulated manner and at levels which are similar to fresh islets over a period of three months. These EMPs were also reported to have become readily vascularized after being transplanted into adequate hosts.
Remarkably, for the first time, the researchers were able to grow and expand by three- to four-fold functional beta cells in culture. This is a relevant achievement as it will allow an increase in the number of transplantations performed by using fewer donor cells per transplant.
“The micro pancreas aims at solving problems currently associated with transplantation of naked islets. In our system, prior to transplantation, islets are cultured within a biological scaffold that supports their survival, leading to long term functionality of the majority of the cells. This could translate in using a much smaller number of islets, enabling treating a higher number of patients. Furthermore, the fact that we have shown expansion of beta cells in the laboratory while still retaining beta cell functionality is a significant breakthrough that may allow to utilize even less initial donors’ islets to treat individual patients,” Professor Eduardo Mitrani from the Hebrew University, Chairman of Betalin’s Scientific Advisory Board and the developer of the technology, said in a press release. “Our promising data raise the hope that Betalin Therapeutics will significantly improve on current treatments for people suffering from diabetes Type 1, as well as for people with severe, advanced levels of diabetes Type 2.”
“We are currently in the midst of a financing round to support clinical studies towards the completion of the first-in-human trial,” said Mr. Doron Birger, Chairman of the Board of Directors, Betalin Therapeutics. “We are fortunate to have in our scientific advisory board two leading figures in the area of cell transplantation, Prof. Camillo Ricordi, from the Diabetes Research Institute & Cell Transplant Center in Miami, and Prof. James Shapiro, from the University of Alberta in Edmonton, Canada. Backed by these renowned scientists, and in addition to promising experimental results to date, Betalin is well positioned to transform the treatment of diabetes for the benefit of diabetic patients worldwide.”
Added Professor Shapiro: “If Betalin’s new microscaffold technique continues to demonstrate efficacy in vivo, it has the potential to substantially improve cellular engraftment and survival both for islets and potentially for stem cell engraftment in future for clinical application.”


can a person volunteer to do a trial