 The International Union Against Tuberculosis and Lung Disease is concerned about the increase of Diabetes incidences in countries where Tuberculosis (TB) is prevalent, since Diabetes increases the susceptibility for contracting the infection.
The International Union Against Tuberculosis and Lung Disease is concerned about the increase of Diabetes incidences in countries where Tuberculosis (TB) is prevalent, since Diabetes increases the susceptibility for contracting the infection.
Diabetes mellitus, or diabetes, is a chronic disease that develops when the pancreas is not capable of producing or utilizing insulin, a hormone that enables glucose. Glucose is essential to the breakdown of carbohydrates in the system. When these pathological conditions occur, there is high level of glucose in the blood, known as hyperglycemia. High levels of glucose in the blood for long periods are associated with damage and failure of various organs and tissues. In 2013, Diabetes affected 382 million people worldwide, but in 2035, the number is expected to reach 592 million. Most cases of the disease are and will continue to be Type 2 diabetes, which is associated with obesity, due to sedentary lifestyles and Western diets.
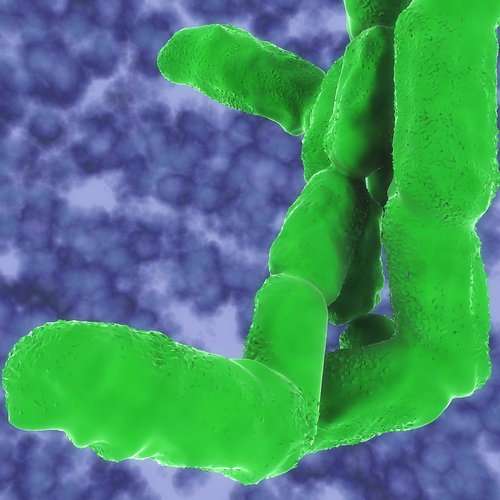
According to the World Health Organization (WHO), last year tuberculosis (TB) was responsible for the death of approximately 1.5 million people. Tuberculosis (TB) is caused by a bacterium called Mycobacterium tuberculosis. The bacteria usually affects the lungs, but can also infect other parts of the body like the kidney, spine, and brain, and if not correctly treated can be fatal. There are two types of TB associated conditions: latent TB infection, where the bacteria can live in the body without causing disease and is not contagious, and TB disease, when the bacteria is multiplying in the body and is transmissible to another individual. Experts are concerned with the possible global rapid increase of cases of tuberculosis if diabetes is not adequately controlled, since this disease is a chronic condition that affects the immune system, and triples increases the risk of a person developing TB. In addition, patients with diabetes will become sick from latent TB infection much more frequently, since their immune systems are compromised, a situation that could lead to an epidemic of co-infection.
This type of co-infection has already occurred in the HIV/AIDS pandemic, an infection that destroys the immune system of an individual, which led to a 4-fold increase of TB rates in many countries in Africa. As a result, clinicians are concerned that this situation will happen with Diabetes as well — mainly in the poorest countries. Although Diabetes is not as big of a threat as HIV infection, since HIV increases the risk of TB 30 times, there are around 10 times more cases of diabetes in the world as people living with HIV, so the total impact is similar.
The greatest increase in Diabetes by 2035 will affect China, India, Brazil, Indonesia, Pakistan, and Russia, 6 out of 10 countries that are classified by the WHO as high TB-burden countries. Dr. Anthony Harries from The International Union Against Tuberculosis and Lung Disease, said to Reuters, that relative to TB, he was particularly alarmed with India and China, as India has the largest percentage of TB cases worldwide, followed by China, whereas for diabetes, China is on top of the list, followed by India. Dr. Anthony Harries also added that, “We want to raise an alarm that we don’t watch history repeat itself with TB-diabetes.” “If we don’t act now to head this off, we’re going to experience a co-epidemic of TB-diabetes that will impact millions and sap public health systems of precious resources. The key is to prevent this from happening,” said Dr. Anil Kapur of the World Diabetes Foundation.
At a recent international lung conference in Barcelona, the research groups of Dr. Harries and Dr. Kapur presented a report calling for a concerted international effort to combat this alarming co-epidemic. The report challenges the conventional approach of taking care of infectious diseases, like TB, and chronic non-communicable diseases, such as Diabetes, independently and not in a combined manner. Finally, the report highlights that this threat needs to be tackled using a strategy of screening both patients with Diabetes for TB and vice-versa, as well as treating both diseases. Unfortunately, this “bi-directional” approach is currently inconsistent in global healthcare.