Evidence from a recent study shows that human umbilical cord mesenchymal stromal cells (hUC-MSCs), when isolated from women with gestational diabetes, display premature aging, poorer cell growth, and altered metabolic function. The study is entitled, “Umbilical Cord Mesenchymal Stromal Cells Affected by Gestational Diabetes Mellitus Display Premature Aging and Mitochondrial Dysfunction,” and is published in the current issue of the journal Stem Cells and Development.
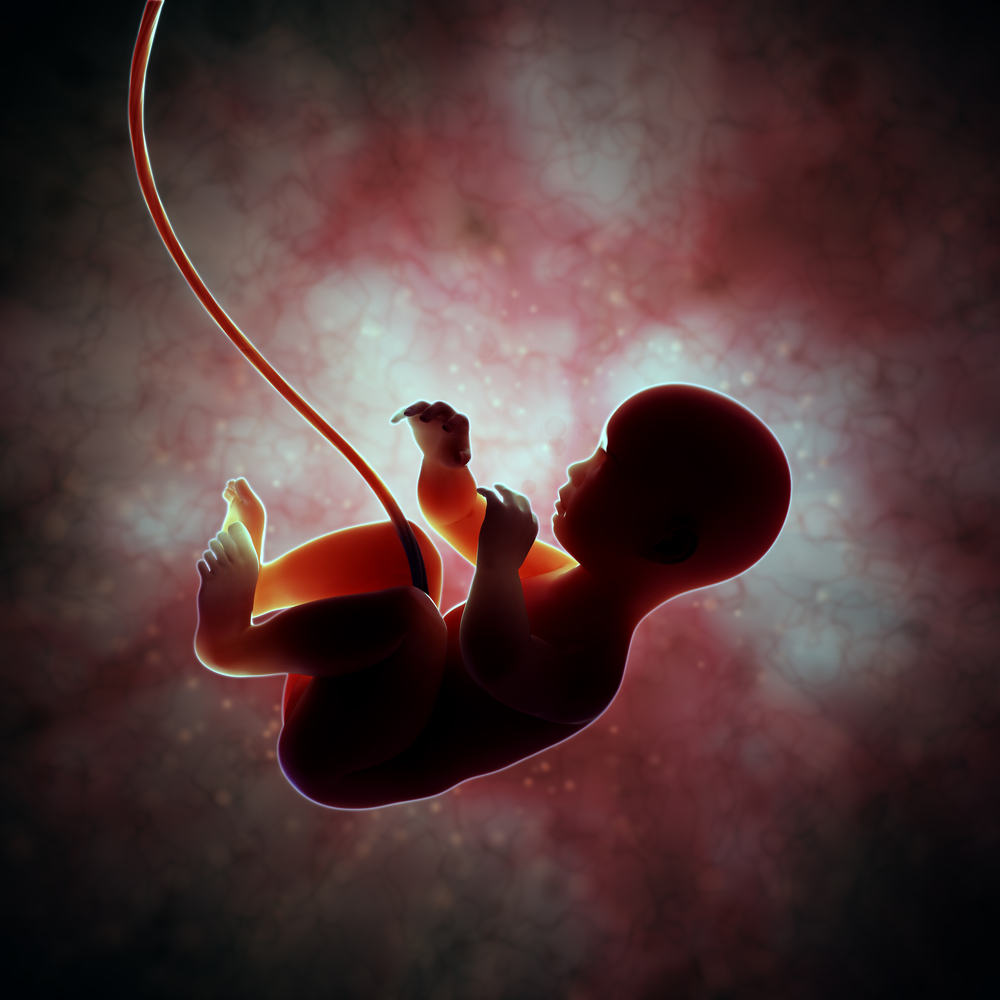
Human umbilical cord mesenchymal stromal cells of Wharton’s jelly origin undergo adipogenic, osteogenic, and chondrogenic differentiation in vitro. Evidence from recent studies shows that these cells have the potential to be used in the development of therapeutics in human disease models of various conditions. However, the biological effects of major pregnancy complications on the cellular properties of hUC-MSCs remain poorly understood.
To help find answers to this question, Jene Choi, PhD from the Department of Pathology Asian Medical Center, University of Ulsan College of Medicine in Korea, and colleagues compared the basic properties of hUC-MSCs obtained from gestational diabetes mellitus (GDM) patients (GDM-UC-MSCs) with those obtained from normal pregnant women (N-UC-MSCs). Choi’s team examined cell growth, cellular senescence, and mitochondrial gene expression (MSC) to assess metabolic activity.
Data analysis revealed that, when compared to N-UC-MSCs, GDM-UC-MSCs revealed decreased cell growth, earlier cellular senescence, and lower osteogenic and adipogenic differentiation potentials. The results also revealed that the GDM-UC-MSCs exhibited little mitochondrial activity and significantly reduced expression of specific genes that regulate mitochondrial function.
The researchers concluded that maternal metabolic imbalance during gestation affects the natural properties of fetal cells. These findings also highlight the significance of the need to adequately assess pregnant women for any other health conditions that may pose a threat to the unborn child’s developing cells.
“We are only just beginning to scratch the surface of understanding how environmental and gestational stressors of all kinds affect stem cell populations,” said Editor-in-Chief Graham C. Parker, PhD, The Carman and Ann Adams Department of Pediatrics, Wayne State University School of Medicine, Detroit, MI, in a recent news release, “The work described offers a non-invasive assay to help determine risk of developmental clinical vulnerability.”
In other developments in diabetes, a temporary tattoo innovatively designed to extract and measure the levels of glucose in the fluid stored in between skin cells has been tested by nanoengineers at the University of California, San Diego. This is the first-ever example of the easy-to-wear and flexible device, and could be a huge step towards noninvasive glucose testing for patients living with diabetes.