Scientists have found a way to convert human skin cells into completely functional pancreatic cells able to produce insulin in response to changes in the levels of glucose, and which, when transplanted into mice, were able to keep the animals from developing diabetes, a new study reported.
The important study, “Human pancreatic beta-like cells converted from fibroblasts,” was conducted by a team of researchers from the Gladstone Institutes and the University of California, San Francisco (UCSF), and published in the journal Nature Communications.
The generation of functional pancreatic insulin-producing beta cells for the effective treatment of diabetes is a key area of translational research.
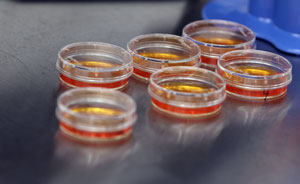
The team used genetic and pharmaceutical molecules to reprogram skin cells into endoderm progenitor cells, and stimulated these endoderm cells to divide quickly, allowing over a trillion-fold expansion. The cells, importantly, did not exhibit any tumor development evidence, and kept their individuality as early organ-specific cells. They developed into pancreatic precursor cells, and were then converted into fully functional pancreatic beta cells. These fully functional pancreatic beta cells were found to protect mice from developing diabetes, as they were capable of producing insulin in response to alterations in the levels of glucose.
“Our results demonstrate for the first time that human adult skin cells can be used to efficiently and rapidly generate functional pancreatic cells that behave similar to human beta cells,” said Dr. Matthias Hebrok, director of the Diabetes Center at UCSF and co-senior author of the study, in a news release. “This finding opens up the opportunity for the analysis of patient-specific pancreatic beta cell properties and the optimization of cell therapy approaches.”
The breakthrough findings represent an important advance in cellular reprogramming technology, allowing researchers to successfully scale-up the production of pancreatic cells, as well as manufacture trillions of the target cells in a systematic and accurate way. It also unlocks the prospect for disease modeling and medicine assessment, and moves diabetic patients closer to tailored cell treatments.
“This study represents the first successful creation of human insulin-producing pancreatic beta cells using a direct cellular reprogramming method,” said the study’s first author, Dr. Saiyong Zhu, a postdoctoral researcher at the Gladstone Institute of Cardiovascular Disease. “The final step was the most unique — and the most difficult — as molecules had not previously been identified that could take reprogrammed cells the final step to functional pancreatic cells in a dish.”
Dr. Sheng Ding, a senior investigator in the Roddenberry Stem Cell Center at Gladstone and co-senior author on the study, added, “This new cellular reprogramming and expansion paradigm is more sustainable and scalable than previous methods. Using this approach, cell production can be massively increased while maintaining quality control at multiple steps. This development ensures much greater regulation in the manufacturing process of new cells. Now we can generate virtually unlimited numbers of patient-matched insulin-producing pancreatic cells.”