 Both type-1 and type-2 diabetes, the two major forms of diabetes, may be the result of the same mechanism after all, according to a study conducted at the Universities of Manchester and Auckland and recently published at the FASEB Journal. After 20 years of work in New Zealand, scientists have reached the conclusion that both types could be slowed down and potentially reversed by drugs that stop the hormone amylin from forming “toxic clumps” in the body.
Both type-1 and type-2 diabetes, the two major forms of diabetes, may be the result of the same mechanism after all, according to a study conducted at the Universities of Manchester and Auckland and recently published at the FASEB Journal. After 20 years of work in New Zealand, scientists have reached the conclusion that both types could be slowed down and potentially reversed by drugs that stop the hormone amylin from forming “toxic clumps” in the body.
Professor Garth Cooper from The University of Manchester studied amylin, which like insulin is produced by cells in the pancreas, in collaboration with his University of Auckland-based research team. Dr. Cooper determined that when insulin and amylin don’t work together normally to regulate the body’s response to food intake, the levels of sugar in the blood rise, causing diabetes and damaging organs as the heart, kidneys, eyes, and nerves.
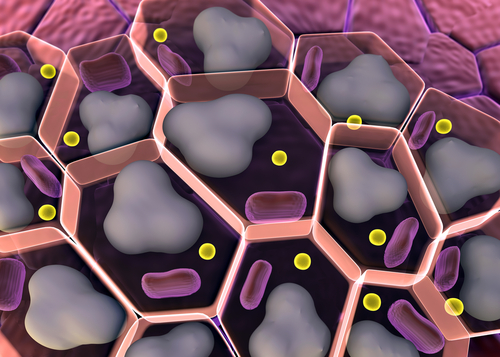
Amylin can, on the other hand, be deposited around cells in the pancreas, creating toxic clumps and demolishing the cells, which would normally produce insulin and amylin. This chain reaction causes a vicious cycle, and if these cells die, it can cause diabetes. Previous research conducted by Professor Cooper had already studied this process in type-2 diabetes. However, this new research is the first of its kind to establish that both types result from the same causative mechanism.
While in type-1 diabetes the process happens faster and starts at an earlier age, given the more rapid deposition of toxic amylin clumps in the pancreas, in type-2 diabetes, the process is the same, but happens at a different rhythm, as suggested by the research. The scientific team will now advance into clinical trials in the next two years in order to assess potential medicines. The trials are being planned with research groups in both England and Scotland, and will include type-1 and type-2 diabetic patients.
The work, entitled “The pathogenic mechanism of diabetes varies with the degree of over expression and oligomerization of human amylin in the pancreatic islet beta cells,” was supported by the Endocore Research Associates University of Auckland, New Zealand, the New Zealand Ministry of Business, Innovation and Employment, the Health Research Council of New Zealand, the Maurice Wilkins Centre, and The University of Manchester, Central Manchester University Hospitals NHS Foundation Trust and the Medical Research Council.