A multi-institutional team of researchers led by senior investigator Fumihiko Urano, MD, PhD, of Washington University School of Medicine in St. Louis (WUSTL) have discovered that a commonly prescribed muscle relaxant drug may also be effective as a treatment for a rare but particularly devastating form of diabetes.
A multi-institutional team of researchers led by senior investigator Fumihiko Urano, MD, PhD, of Washington University School of Medicine in St. Louis (WUSTL) have discovered that a commonly prescribed muscle relaxant drug may also be effective as a treatment for a rare but particularly devastating form of diabetes.
The drug, Dantrolene, is used to treat spasticity or muscle spasms associated with spinal cord injuries, stroke, multiple sclerosis, cerebral palsy, and other conditions. However, the research team found it also prevents destruction of insulin-producing beta cells in both animal models of Wolfram syndrome, and in cell models derived from patients with the illness.
Results of the study were published Nov. 24 in the Proceedings of the National Academy of Sciences (PNAS) Online Early Edition. The paper, entitled “A calcium-dependent protease as a potential therapeutic target for Wolfram syndrome“ (PNAS Online Early Edition, Nov. 24, 2014 ).
The coauthors describe Wolfram syndrome as an autosomal recessive disorder characterized by juvenile diabetes and neurodegeneration, and considered a prototype of human endoplasmic reticulum (ER) disease. Persons with Wolfram syndrome typically develop type 1 diabetes in very early childhood and will require insulin injections several times daily. Other symptoms associates with the syndrome include hearing loss, optic nerve atrophy and balance difficulties due to neurodegeneration. Many Wolfram syndrome patients die by age 40.
They explain that Wolfram syndrome is a consequence of loss of function mutations of two causative genes — Wolfram syndrome 1 (WFS1) and Wolfram syndrome 2 (WFS2) — which encode transmembrane proteins localized to the ER.
The coauthors note that while it is extremely rare (affecting just one in 500,000 people worldwide), Wolfram syndrome presents the best human disease model currently available for identifying drugs and biomarkers associated with ER health. Moreover, Wolfram syndrome is ideal as a medium for studying mechanisms of ER stress-mediated death of neurons and cells.
In their paper, the researchers identify elevated levels of the enzyme calpain 2 as the main cause of brain cell and insulin-producing cell death in Wolfram syndrome, based on their finding that pathways leading to calpain activation offer potential drug targets for Wolfram syndrome and that substrates for calpain might serve as biomarkers for the syndrome. They discovered that Dantrolene blocks cal pain and also prevents brain cell death in both animal and cell models of the disorder. They conclude that their results demonstrate that calpain and the pathway leading its activation provides potential therapeutic targets for Wolfram syndrome and other ER diseases.
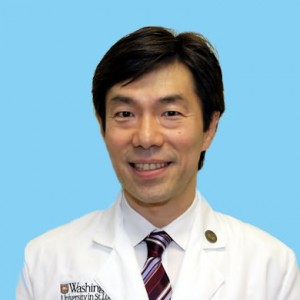 “Because the drug is approved by the Food and Drug Administration (FDA), clinical trials in Wolfram patients could get underway relatively quickly, says senior investigator Fumihiko Urano, MD, PhD, a renowned diabetes researcher who was last year named the new Samuel E. Schechter Professor of Medicine at Washington University School of Medicine in St. Louis.
“Because the drug is approved by the Food and Drug Administration (FDA), clinical trials in Wolfram patients could get underway relatively quickly, says senior investigator Fumihiko Urano, MD, PhD, a renowned diabetes researcher who was last year named the new Samuel E. Schechter Professor of Medicine at Washington University School of Medicine in St. Louis.
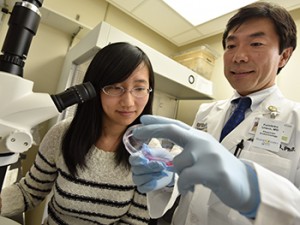
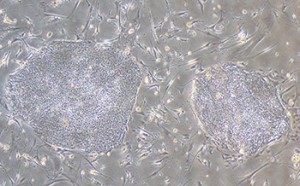
Dr. Urano’s research at WUSTL involves locating biomarkers that may lead to more effective treatments, or even a cure, for juvenile-onset diabetes, including Wolfram syndrome. HIs lab’s central research focus is on developing personalized medicine for juvenile diabetes and genetic forms of diabetes, especially Wolfram syndrome, by using induced-pluripotent stem cells (iPS cells) derived from patients’ skin cells. His team is also developing a method for the regeneration of insulin-producing cells using a trophic factor. “We’d like to test the drug first in adult patients with Wolfram syndrome, and if we get positive results, we could extend the trial to children,” Dr. Urano says in a WUSTL release.
Dantrolene often is prescribed to people with cerebral palsy or multiple sclerosis to treat muscle spasticity. If proven effective in patients with Wolfram syndrome, it’s possible that it could also be a viable treatment for patients with the more common forms of diabetes since Calpain 2 is overactive in cell models of those variants as well. One potential downside of Dantrolene treatment is that it can cause severe liver damage.
The WUSTL release also reports that as part of their study of treatment targets for Wolfram syndrome, Dr. Urano and his research team have additionally studied Dantrolene’s effects of on stem cells taken from Wolfram syndrome patients and their close relatives, such as parents or siblings. They note that unlike adult stem cells collected from cord blood or stem cells developed from embryos, the stem cells examined in these studies were grown from donor skin cells, and treated with growth factors so they would differentiate into specific cell types, such as neurons and insulin-producing cells.
Cells from Wolfram patients themselves produced high levels of calpain 2 leading to cell death. However, when the researchers treated those cells with Dantrolene, they report that everything changed. Calpain 2 level dropped, and cells stopped dying. “We also found that dantrolene was not toxic to cells grown from the skin samples donated by patients relatives,” Dr. Urano observes. “The drug interfered with cell death in cells from Wolfram patients but did not harm cells that came from parents and siblings.”
These finding lead the researchers to hope that Dantrolene may also prove effective against the more common type 1 and type 2 diabetes.
“Wolfram is the most difficult form of diabetes because these patients have problems with blood sugar and so many other challenges,” Dr. Urano explains. “Calpain 2 also plays a role in type 1 and type 2 diabetes. Currently, we are studying the drug in animal and cell models of those types of diabetes to see if it also keeps insulin-producing cells from dying.”
Having established that Dantrolene can prevent the death of brain cells and of insulin-secreting beta cells in Wolfram syndrome, Dr. Urano wants to next investigate more closely at how the drug affects other tissues, including the eye in studies slated to begin soon.
The research is funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) at the National Institutes of Health (NIH), the Juvenile Diabetes Research Foundation, the American Diabetes Association, Team Alejandro, Team Ian, the Ellie White Foundation for Rare Genetic Disorders and the Jack and J.T. Snow Scientific Research Foundation. NIH grant numbers are DK067493, P60 DK020579 and UL1 TR000448.
Sources:
Washington University School of Medicine in St. Louis
Proceedings of the National Academy of Sciences (PNAS)
Image Credits:
Robert Boston
Urano Lab
Note: The study above was coauthored by Fumihiko Urano, Kohsuke Kanekura, Takashi Hara, Jana Mahadevan, Larry D. Spears, Cris M. Brown, and Clay F. Semenkovich of the Department of Medicine, Division of Endocrinology, Metabolism, and Lipid Research, Washington University School of Medicine, St. Louis; Simin Lua of the Graduate School of Biomedical Sciences, University of Massachusetts Medical School, Worcester, MA; Christine M. Oslowski of the Department of Medicine, Boston University School of Medicine, Boston; Rita Martinez, Amber Neilson, and Patrick Blanner of the Department of Genetics, iPSC core facility, Washington University School of Medicine, St. Louis; Mayu Yamazaki-Inoue, Masashi Toyoda, and Akihiro Umezawa of the Department of Reproductive Biology, National Center for Child Health and Development, Tokyo, Japan; Bess A. Marshall of the Department of Pediatrics, Washington University School of Medicine, St. Louis; Tamara Hershey of the Departments of Psychiatry, Neurology, and Radiology, Washington University School of Medicine, St. Louis; Peter A. Greer of the Department of Pathology and Molecular Medicine, Queen’s University, Division of Cancer Biology and Genetics, Queen’s Cancer Research Institute, Kingston, Ontario, Canada.